Governor Signs Bill to Reform Indiana’s Medicaid Program

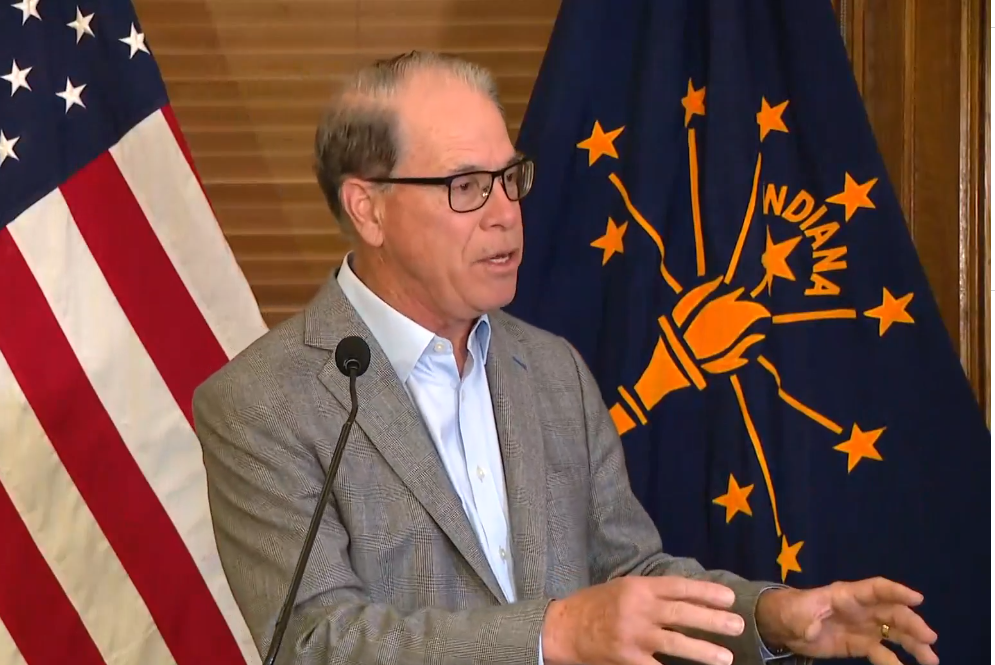
INDIANAPOLIS, IN – A new law signed by Governor Mike Braun is poised to address the rising costs of Indiana’s Medicaid program and provide greater support for families with medically complex patients.
The legislation, House Enrolled Act 1689, co-authored by State Representative Bob Behning, will promote transparency and data collection within the Family and Social Services Administration (FSSA) to ensure the state is efficiently using its resources.
The bill’s passage comes after a period of unsustainable growth in Medicaid spending, driven in part by expanded access to home- and community-based services during the pandemic. This surge led to a waitlist for the Health and Wellness waiver, leaving many families in limbo, particularly those who had relied on a parent or guardian to serve as a compensated caregiver.
“Our Medicaid costs continue to take up more and more of the state budget, straining important programs and leading to waitlists for Hoosier families needing these services,” said Behning. “This law aims to identify long-term solutions to ensure we are providing support to those who need it most while reforming Medicaid to combat rising, unsustainable costs.”
One of the key provisions of HEA 1689 is to establish a dialogue between the FSSA and the Division of Disability and Rehabilitative Services Advisory Council.
Their goal is to propose a state plan amendment that could re-introduce the “Legally Responsible Individual” language to the Health and Wellness waiver, but in a more cost-effective manner. The law also shifts oversight of the H&W and Traumatic Brain Injury waivers to the Bureau of Disability Services Ombudsman program to improve service delivery and better address the underutilization of services.
Additionally, the legislation enhances reporting and data collection by the FSSA, which will help identify gaps in services and improve the overall quality of care for vulnerable Hoosiers.
The new law is seen by lawmakers as a crucial step toward ensuring the long-term sustainability of the state’s Medicaid program.